SPRINT PNS System
Clinically proven pain relief
In clinical studies, the vast majority of SPRINT PNS patients reported significant and sustained relief of pain and/or pain interference.1-5, 7-11,^
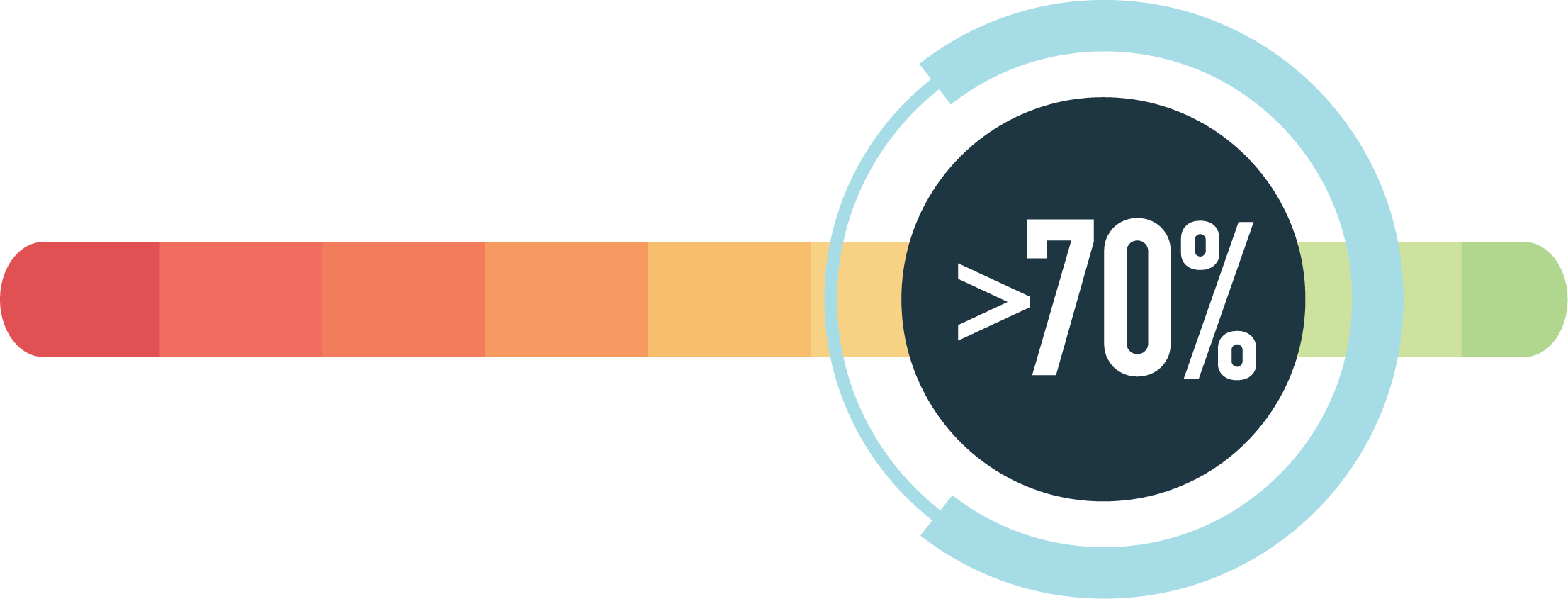
Backed by the largest review of real-world PNS data
The largest retrospective review of real-word PNS data of over 6,100 patients, with over 71% demonstrating significant pain relief and/or improvement in quality of life following 60-day percutaneous PNS treatment with the SPRINT PNS System.12,†,‡
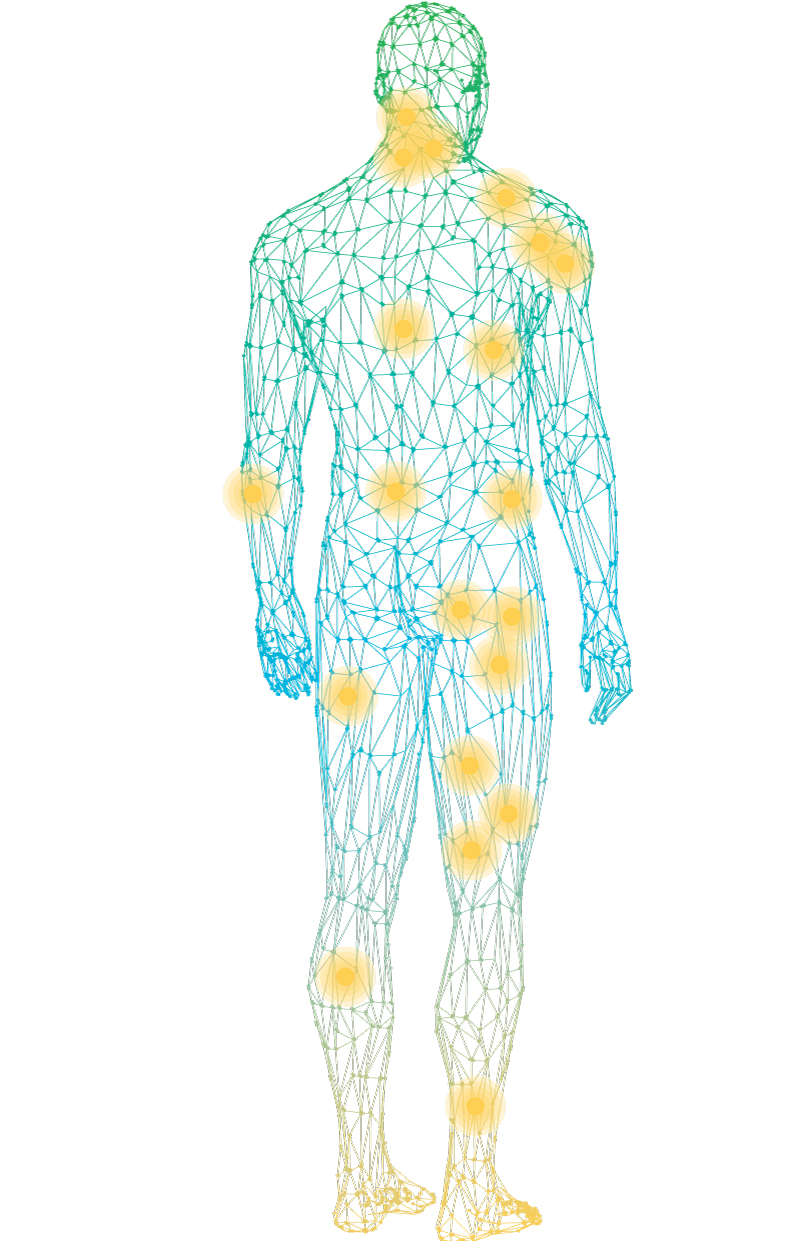
Head-to-toe Treatment Options™
SPRINT PNS may be a solution for a wide variety of moderate-to-severe pain conditions, including:
The SPRINT PNS System is not intended to be placed in the region innervated by the cranial and facial nerves.
First-Line PNS™ treatment
The SPRINT PNS System is a patient-preferred**, low risk alternative to more invasive treatments such as ablation, permanent implants, or surgery. Our breakthrough First-Line PNS treatment is shown to provide significant and sustained pain relief in clinical studies when prior treatments such as opioids or injections have failed.
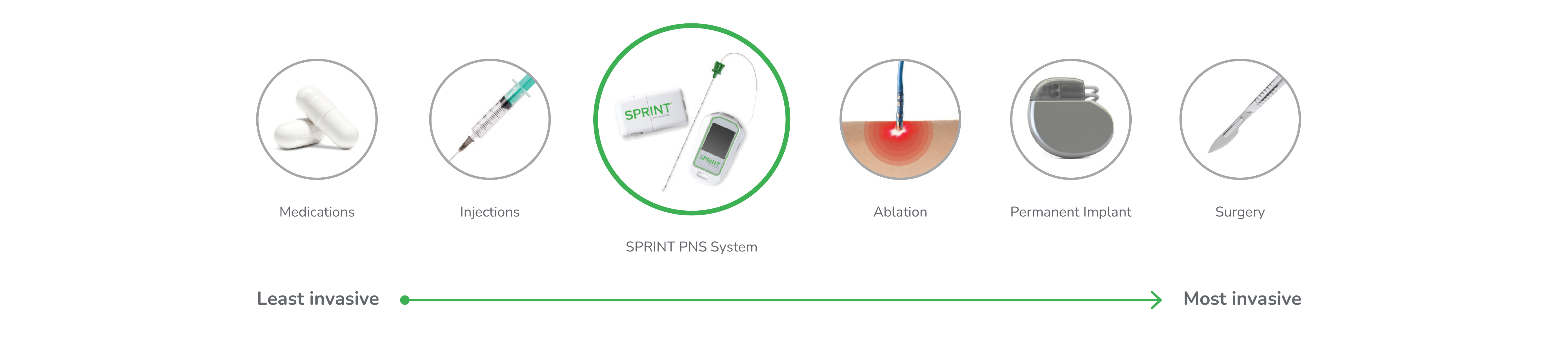
Patient-preferred** treatment
As the least invasive implantable PNS available, the SPRINT PNS System delivers the approach to pain relief patients prefer.
Smallest diameter PNS lead available
60-day PNS (e.g. SPRINT PNS System) preferred by patients to radiofrequency ablation
Only FDA-cleared implantable PNS system that does not require incisions or a permanent implant
^In clinical studies, the most common adverse events were skin irritation and erythema.
†The total rate of medical events collected from the product complaint database was approximately 6%, with skin irritation due to adhesive components as the most reported event.
‡Significant pain relief and/or improvement in quality of life defined as ≥ 50% pain relief and/or at least Minimally Improved on PGIC.
**In a market research study, SPRINT PNS was a patient-preferred treatment.13
References
- Chae J, et al. Am J Phys Med Rehabil. 2005;84(11): 832-842.
- Gilmore C, et al. Pain Pract. 2020;20(3):310-320.
- Gilmore C, et al. Reg Anesth Pain Med. 2020;45(1):44-51.
- Gilmore C, et al. Interv Pain Med. 2023;2:100243.
- Goree JH, et al. Neuromodulation. 2024;27:847861.
- Gilmore et al. ASPN Poster 2024.
- Yu D, et al., Arch Phys Med Rehabil. 2001;82(1):20-25.
- Chae J, et al. Pain Pract. 2013;13(1):59-67.
- Rauck RL, et al. Neuromodulation. 2014;17(2):188-197.
- Wilson RD, et al. Am J Phys Med Rehabil. 2014;93(1):1728.
- Wilson RD, et al. Neuromodulation. 2014;17(8):771-776.
- Huntoon M, et al. Pain Phys. 2023;26:273-281.
- Staats P, et al. Pain Mgmt. 2021;12(3):371-382.