Clinical Evidence
Published or ongoing prospective clinical studies1-18
Peer-reviewed publications
DoD and NIH funding to support research
Randomized controlled trials (RCTs)
SPRINT PNS is supported by clinical data from 7 successful RCTs, which have demonstrated clinically significant improvements in pain, functional outcomes, medication usage, and/or quality of life across a variety of pain conditions, such as:
- Shoulder Pain3, 5
- Post-Amputation Pain12, 15
- Post-Surgical Pain 14, 17
- Low Back Pain19
Real-world evidence
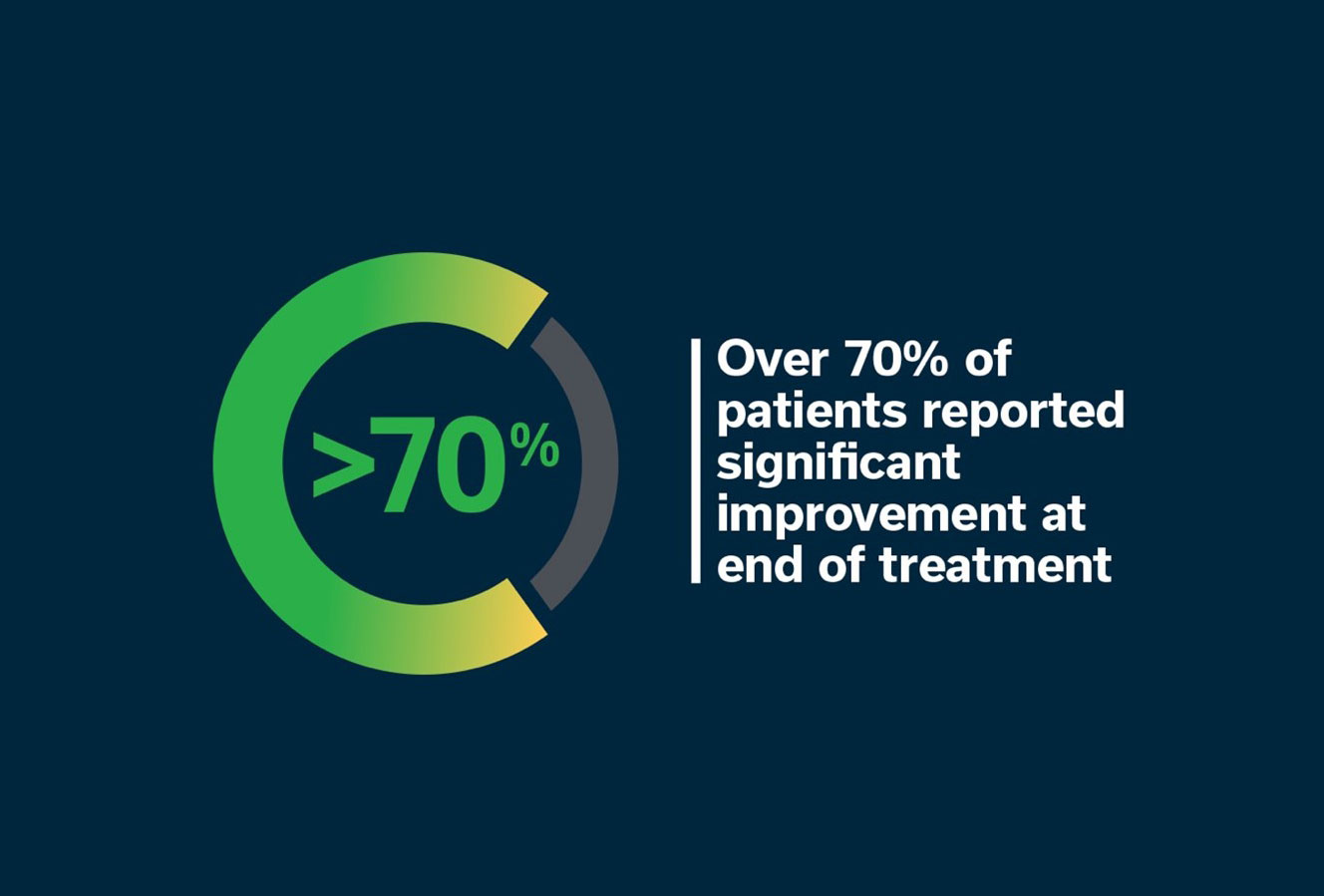
The largest retrospective review of real-word PNS data of over 6,100 patients, with over 71% demonstrating significant pain relief and/or improvement in quality of life following 60-day percutaneous PNS treatment with the SPRINT PNS System.20*
*The total rate of medical events collected from the product complaint database was approximately 6%, with skin irritation due to adhesive components as the most reported event.
References
- Yu D, et al. Arch Phys Med Rehabil. 2001; 82(1): 20-25.
- Renzenbrink G, et al. Clin Rehabil. 2004; 18(4): 359-365.
- Chae J, et al. Am J Phys Med Rehabil. 2005; 84(11): 832-842.
- Chae J, et al. Pain Pract. 2013; 13(1): 59-67.
- Wilson R, et al. Am J Phys Med Rehabil. 2014; 93(1): 17-28.
- Wilson R, et al. Neuromodulation. 2014; 17(8): 771-776.
- Rauck R, et al. Neuromodulation. 2014; 17(2): 188-197.
- Ilfeld B, et al. Pain Pract. 2017; 17(7): 892-901.
- Ilfeld B, et al. J Orthop Surg Res. 2017; 12(1): 4.
- Wilson R, et al. Neuromodulation. 2018; 21(3): 290-295.
- Ilfeld B, et al. Neuromodulation. 2019; 22(5): 653-660.
- Gilmore C, et al. Neuromodulation. 2019; 22(5): 615-620.
- Gilmore C, et al. Reg Anesth Pain Med. 2020; 45(1): 44-51.
- Ilfeld B, et al. Anesthesiology. 2021; 135: 95–110.
- Albright-Trainer B, et al. Pain Mgmt. 2022; 12(3): 357-369.
- Gilmore C, et al. Interv Pain Med. 2023; 2(2): 100243.
- Goree J, et al. Neuromodulation. 2024; 27(5): 47-861.
- Ongoing studies listed on ClinicalTrials.gov as of January 21, 2025.
- McCormick Z, et al. Poster from NANS Annual Meeting 2025.
- Huntoon M, et al. Pain Physician. 2023; 26: 273-281.